Health and Learning Are Deeply Interconnected in the Body: An Action Guide for Policymakers
We know that adult-child relationships, other early experiences, and environmental exposures influence child well-being. An increasing number of policies and programs around the world now reflect that understanding by supporting children’s early learning and nutrition to improve their readiness to succeed in school. As scientific knowledge continues to grow, we also know more clearly than ever how the conditions and environments in which children develop affect lifelong health as well as educational achievement.
Three key messages from this science can help guide our thinking in a time when innovation has never been more needed in public systems in order to improve both health and learning.
#1: The brain and all other systems in the body interact with each other as they adapt to the environment.
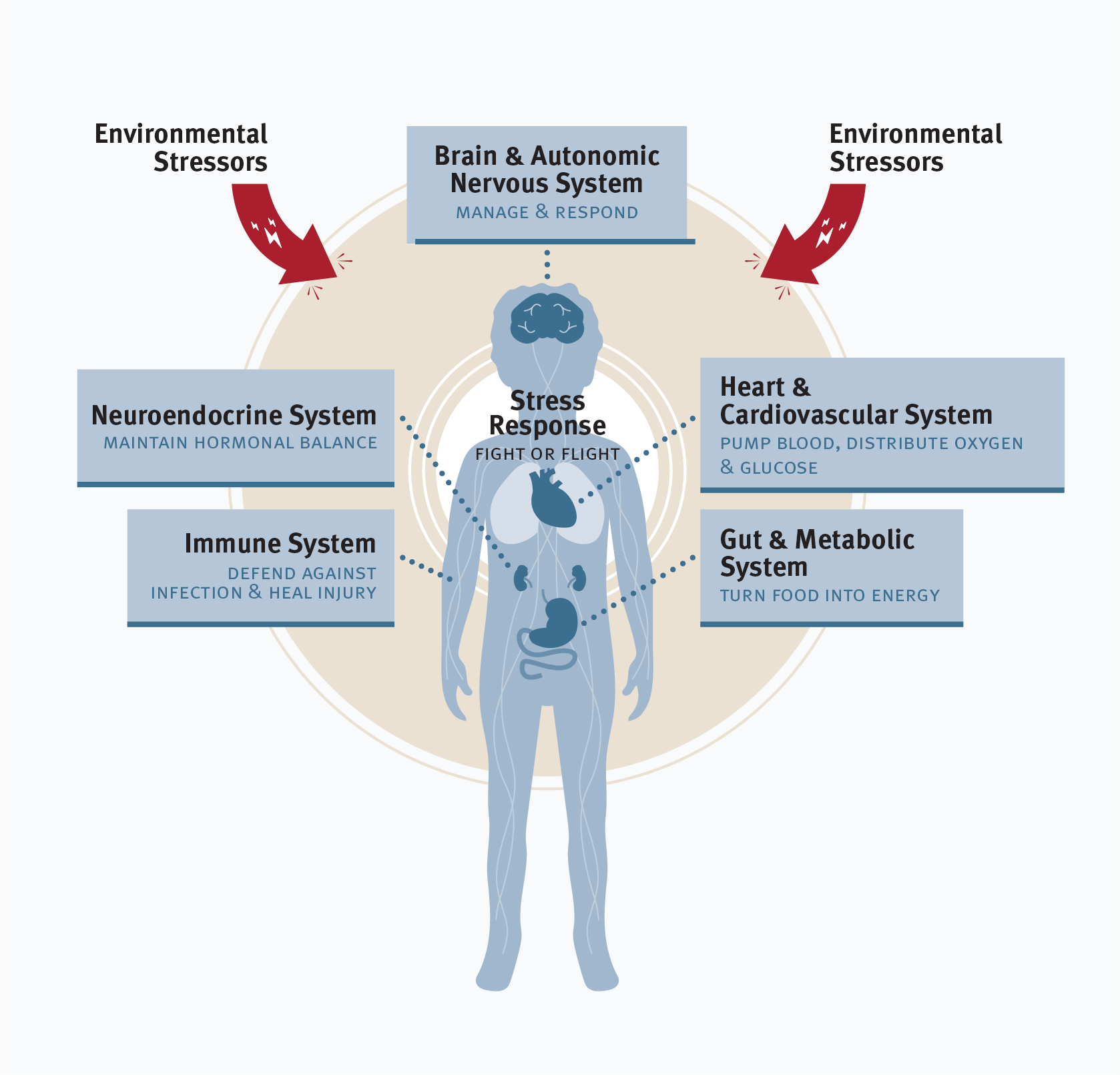
The conditions we create and the experiences we provide for young children affect not just the developing brain, but also other systems in the body, including immune responses and metabolic regulation. Working like a team of skilled athletes, these systems rely on and react to information from the environment and from each other. Together, they perform the functions that are essential for lifelong well-being. Implications: Because all biological systems in the body are connected, supporting families with young children and strengthening responsive relationships not only build a foundation for social-emotional development, school readiness, and future learning; they also strengthen the building blocks for a lifetime of physical and mental health.
#2: Experiences during the prenatal period and first 2-3 years after birth affect lifelong health at least as much as they affect school achievement.

Developmental timing is critical. Science tells us that experiences and exposures during pregnancy and the first few years after birth affect developing biological systems in many ways that are difficult to change later. For example, if a woman experiences excessive stress, poor nutrition, or toxic environmental exposures during pregnancy, it can affect how organs, stress response, and metabolic systems develop, with long-lasting impacts into adulthood, such as increased risk for heart disease, obesity, diabetes, and mental health conditions. Implications: Policies and programs that reduce stress, prevent toxic exposures, and provide support for pregnant mothers and families with infants and toddlers will result in better health outcomes across the lifespan and save billions in health care costs. Taken another way, if we delay early investments until later in the preschool period, we will miss a critical opportunity to build a stronger foundation for a healthier and more productive adult population.
#3: Inflammation, as part of the body’s stress response, helps defend against infection, injury, and acute threat—but persistent inflammation in response to chronic adversity can have long-term, disruptive effects on physical and mental well-being.
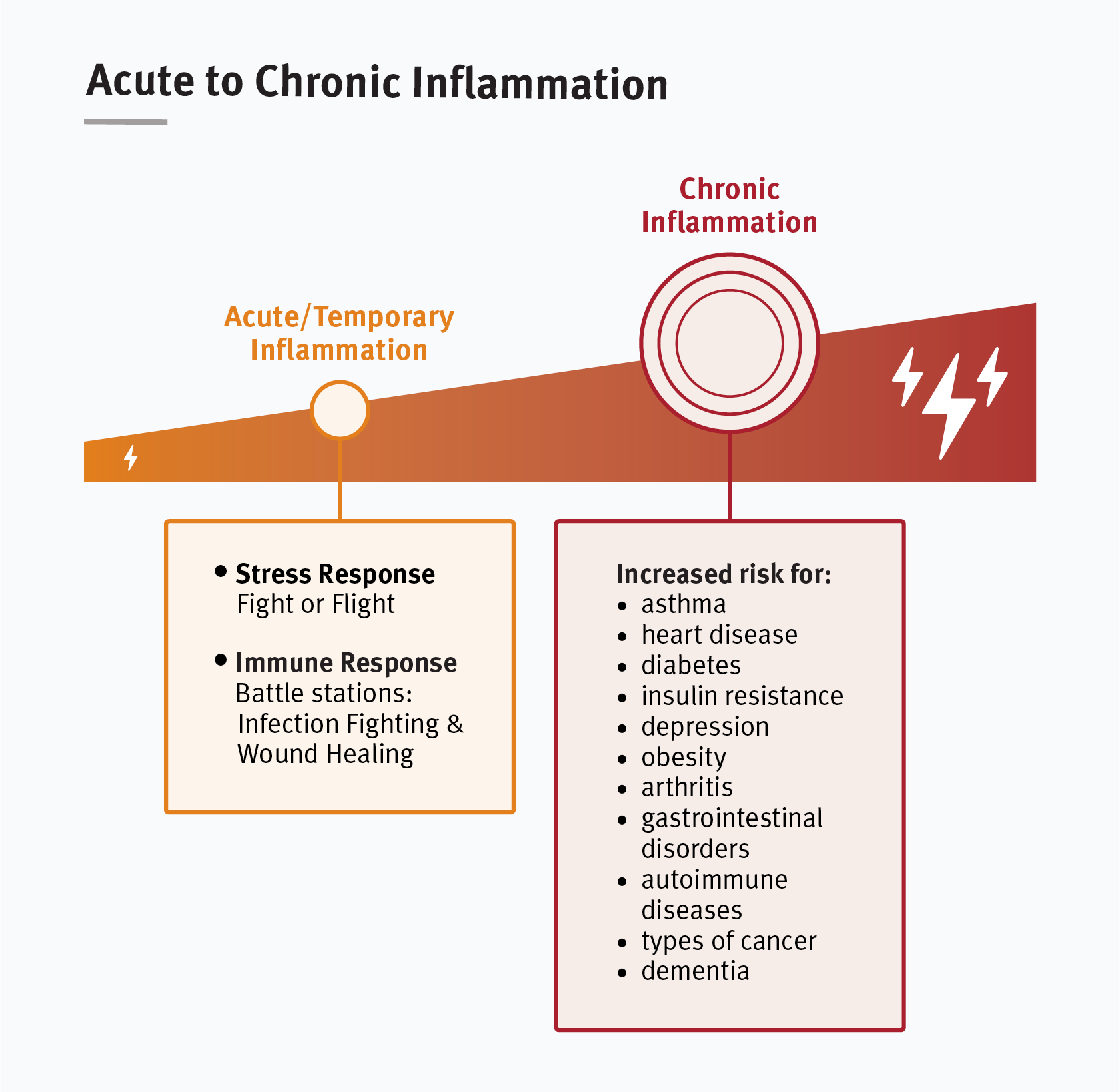
Experiencing persistently adverse environments very early in childhood may produce chronic inflammatory conditions that can last for a lifetime, including heart disease, diabetes, depression, arthritis, gastrointestinal disorders, autoimmune diseases, multiple types of cancer, and dementia, among many others. Implications: If policies and services can reduce sources of ongoing, excessive stress for young children and their families—such as poverty, racism, violence, housing instability, and food insecurity—we can dramatically reduce the need for costly treatments for a wide range of health conditions. Heart disease, diabetes, and depression alone cost the U.S. more than $600 billion each year and are three of the conditions most likely to be linked to early adversity.
How can this knowledge help us develop more effective policies and programs?
We can confront poverty, racism, violence, housing instability, food insecurity, and other sources of fear and social isolation that impose significant burdens on families raising young children. Evidence-based interventions that build resilience in both children and caregivers can lead to better individual outcomes at a program level, but improving health and learning outcomes across the full population will require more effective, “upstream” efforts to address structural inequities (e.g., unequal access to high-quality education, health care, housing, employment opportunities, and wealth creation) at a societal level.
We can use three science-based principles as a lens for redesigning systems that serve children and the adults who care for them. Policies and programs will be more effective if they:
Support responsive relationships, which are necessary for building sturdy brain architecture, buffering children from excessive stress, and strengthening the building blocks of resilience, all of which support healthy development.
Reduce sources of stress, which will lessen the toll of adversity on health and well-being and make it easier for adults to provide protective relationships for young children.
Strengthen core skills, which adults need for health-promoting behaviors like setting and meeting goals, managing their emotions and behavior, creating daily family routines, and supporting children’s development of these same capacities.
We can strengthen community-based networks among services for families, primary health care for children and their caregivers, and early care and education programs in a seamless ecosystem. Promising models for integrated systems are led by teams that include child development expertise, reflect the cultural and linguistic characteristics of the community they serve, and link services across sectors. Connecting primary care pediatrics more seamlessly to other early childhood systems will require significant changes in health care reimbursement, professional training, and measurement capacity.
For further reading, see the full working paper on which this brief is based.